Atopic dermatitis, the most common form of eczema, affects an estimated 204 million people worldwide, representing approximately 2.6% of the global population. Global Epidemiology of Atopic Dermatitis, British Journal of Dermatology. [1]
This chronic inflammatory skin condition, known as Eczema, is characterized by epidermal barrier impairment, xerosis, pruritus, and recurrent inflammatory flares driven by both environmental and immunological factors. As interest in natural, non-invasive therapies supporting skin health increases, Red Light Therapy has emerged as a photobiomodulation-based approach with substantial effects on cellular function and inflammatory signaling.
Red Light Therapy operates through absorption of red and near-infrared wavelengths by intracellular chromophores, most notably cytochrome c oxidase, a key enzyme within the mitochondrial electron transport chain. This photonic absorption enhances mitochondrial respiration and increases adenosine triphosphate (ATP) production, supplying energy necessary for keratinocyte repair, lipid synthesis, and barrier restoration. Red Light Therapy has repeatedly proven to reduce reactive oxygen species (ROS) accumulation and modulate inflammatory pathways, including down-regulation of NF-κB–mediated cytokine expression, which plays a central role in inflammation.
These physiological effects support several aspects of eczema-prone skin, including improved barrier integrity, reduced inflammatory activity, and enhanced microcirculation for nutrient delivery and waste clearance. As a simplistic light-based solution, this therapy aligns with evidence-based approaches that aim to address underlying cellular dysfunction contributing to chronic skin irritation.
What Causes Eczema? A Look at the Skin’s Biological Stressors
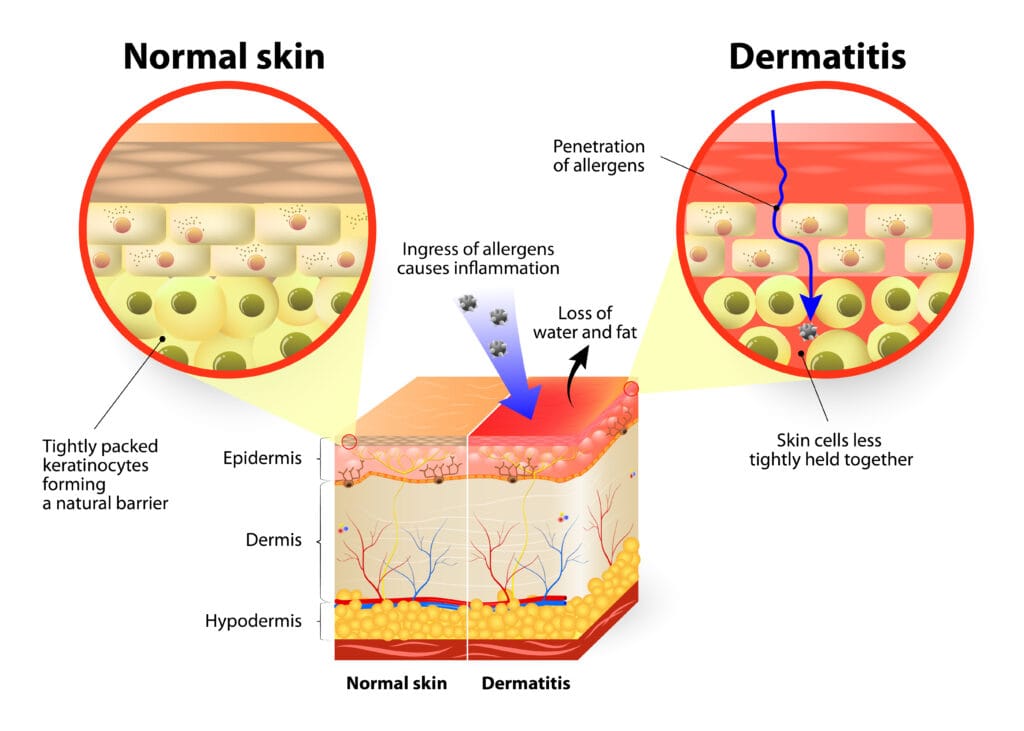
Eczema, particularly atopic dermatitis, develops from a combination of epidermal barrier dysfunction, immune dysregulation, and environmental sensitivity. One of the primary issues is a weakened stratum corneum, the outermost layer of the skin responsible for retaining moisture and shielding against irritants. When this layer becomes compromised, transepidermal water loss increases, leading to dryness, flaking, and heightened sensitivity to environmental triggers.
At the immunological level, eczema is marked by an overactive Type 2 helper T-cell (Th2) response, which elevates inflammatory cytokines such as interleukin-4 (IL-4), interleukin-13 (IL-13), and interleukin-31 (IL-31). These cytokines contribute to redness, itching, and the cycle of inflammation that many victims of Eczema experience. In addition, oxidative stress, often caused by an imbalance of reactive oxygen species, further disrupts the cellular function and can majorly aggravate the skin’s surface.
The skin’s microbiome also plays a role here. Individuals with eczema are more prone to colonization by Staphylococcus aureus, a bacterium known to weaken barrier integrity and stimulate additional immune activity. Combined with factors such as allergens, temperature changes, detergents, or stress, these biological vulnerabilities create conditions that make the skin more reactive and slower to self-repair.

How Red Light Therapy Works at the Cellular Level
Red Light Therapy reinforces eczema-prone skin through photobiomodulation, in which specific red and near-infrared wavelengths have the ability to influence cellular behavior. When these wavelengths reach the skin, they are absorbed by intracellular chromophores, primarily cytochrome c oxidase, a key enzyme within the mitochondrial electron transport chain. This interaction enhances mitochondrial respiration and increases the production of adenosine triphosphate, the molecule responsible for fueling essential cellular functions.
Higher ATP availability enables keratinocytes and fibroblasts, two cell types critical for skin structure and repair, to operate more efficiently. This supports epidermal renewal, barrier restoration, and lipid synthesis, all of which are important for reducing dryness and sensitivity in eczema-prone skin. At the same time, Red Light Therapy helps regulate the skin’s inflammatory response by modulating signaling pathways such as nuclear factor kappa B (NF-κB). This leads to a reduction in pro-inflammatory cytokines that cause redness, irritation, and itch to the skin barrier.
An additional component in cellular targeting is a reduction in reactive oxygen species (molecules that accumulate during inflammation and contribute to oxidative stress). By helping balance ROS (reactive oxygen species) levels, this therapy creates a more stable environment for healthy skin repair. Improvements in microcirculation and lymphatic flow can enhance nutrient delivery and assist in clearing metabolic waste, further supporting skin resilience.
In essence, the cellular effects of Red Light Therapy address many of the underlying factors that contribute to eczema, offering a targeted, science-backed way to promote calmer, healthier skin over time.
Clinical Evidence: Red Light Therapy’s Impact on Eczema-Related Inflammation
While Red Light Therapy, or photobiomodulation (PBM), has not been studied as extensively for eczema as it has for other inflammatory skin conditions, existing clinical evidence across dermatology and oncology provides strong insight into its anti-inflammatory and skin-restorative potential. Much of what is known about light therapy effects on irritated, damaged, or inflamed skin comes from studies examining radiation-induced dermatitis (RID), a condition marked by barrier breakdown, erythema, inflammation, and skin discomfort that shares several pathophysiological features with eczema.
Multiple studies demonstrate that PBM can reduce inflammatory cytokines, support epithelial repair, and improve patient comfort in scenarios where the skin barrier is severely compromised. For example, one case review evaluating light-based therapy for chemoradiotherapy-induced dermatitis reported that “PBM in the anal region during RT treatment enabled symptom relief, radiodermatitis control, and improved the patient’s quality of life. In addition to being an innovative, safe, and low-cost therapeutic option.”[2] (Photobiomodulation as a treatment for dermatitis caused by chemoradiotherapy for squamous cell anal carcinoma: case report and literature review). Although the condition differs slightly from eczema, the inflammatory mechanisms, epidermal injury, cytokine elevation, and impaired repair are biologically the same.
Additional evidence strengthens this pattern. A systematic review assessing acute radiation dermatitis noted that “PBMT may have beneficial effects on the prevention and treatment of higher-grade ARD in patients with breast cancer and head and neck cancer.”[3] (Effects of photobiomodulation therapy for acute radiation dermatitis in patients with cancer: A systematic review and meta-analysis of real-world evidence). These findings show that PBM can support the skin’s ability to modulate inflammation, reduce oxidative stress, and accelerate barrier recovery.
Further research investigating PBM-LED therapy in women receiving adjuvant radiotherapy after breast-conserving surgery found meaningful reductions in skin toxicity, concluding that “PBM-LED therapy applied prior to RT might be effective in decreasing the incidence and sequelae of radiation-induced skin toxicity in breast cancer patients treated with breast-conserving surgery.”[4] (Photobiomodulation therapy for the management of radiation-induced dermatitis: A single-institution experience).
Taken together, these studies highlight PBM’s consistent capacity to reduce inflammation, support skin repair, and protect against barrier damage across diverse clinical settings. Although eczema differs in cause, its symptoms (redness, dryness, irritation, and barrier fragility) stem from similar biological disruptions. Because this therapy works by enhancing mitochondrial function, modulating inflammatory pathways, and improving cellular repair, its benefits in other inflammatory skin conditions provide strong support for its use as a gentle, natural skin-care therapy for those with eczema-prone skin.
Lifelong Benefits of Red Light Therapy for Eczema-Prone Skin
Red Light Therapy presents a non-toxic, clinically proven support system for individuals looking to manage ongoing eczema symptoms and strengthen overall skin health. One of the core advantages of this therapy is its ability to help calm visible irritation. Many users report reduced redness, less itching, and a more balanced appearance after consistent application. With attentive use, the skin begins to function more efficiently, augmenting repair processes, promoting hydration, and reinforcing the skin’s natural barrier. By supporting healthier circulation and overall skin function, Red Light Therapy visibly reduces dryness and sensitivity over time. For individuals who experience frequent flare-ups, these improvements can translate into longer periods of relief and fewer disruptions caused by irritation.
Another practical benefit of light therapy is the cumulative effect of regular use. Because it works in a gentle, non-invasive way, many people have begun incorporating Red Light Therapy into their long-term skincare and wellness routine to help maintain calmer, more resilient skin. With consistent sessions, light therapy supports smoother texture, improved hydration, and a more stable skin environment, factors that are especially important for eczema-prone skin.
To support users in achieving optimal dosing, we encourage the use of our RLT Dose Calculator, which is specifically designed to help users tailor their sessions.
As interest in non-invasive wellness technologies continues to grow, this therapy is becoming an increasingly recognized tool within the broader landscape of skin health. The expanding red light industry reflects a larger shift toward supporting the body’s natural processes rather than relying solely on the common temporary symptom relief modalities. With ongoing advancements and increasing accessibility, Red Light Therapy is positioned to play an even greater role in helping individuals manage eczema and maintain healthier skin in the years ahead.

Advancing Eczema Support With Light-Based Wellness
Eczema affects millions of individuals worldwide, interrupting daily comfort and presenting ongoing challenges related to dryness, irritation, and inflammation of the skin. Traditional approaches often focus on short-term symptom relief, offering temporary comfort without addressing the underlying factors that contribute to skin sensitivity and recurring inflammation. While these methods have their place, many people are seeking options that complement their routine and support the skin in a deeper, more sustained way.
Red Light Therapy stands apart because it works beneath the surface, targeting the biological processes that influence how the skin repairs itself, manages irritation, and maintains resilience over time. Rather than simply masking symptoms, this therapy supports mitochondrial function and increases ATP production, helping keratinocytes and fibroblasts perform essential cellular tasks more efficiently. This cellular support can strengthen the skin barrier, improve hydration, and help moderate inflammatory signaling, all of which are important for those prone to eczema.
By working at this foundational level, Red Light Therapy offers an approach that aligns with the long-term needs of eczema-prone skin: calmer responses to triggers, fewer disruptions caused by inflammation, and better overall skin stability. As understanding of light-based wellness continues to grow, Red Light Therapy has become an accessible and reliable tool for individuals looking to complement their existing skincare routines with a modality that supports the skin’s natural physiology.
With regular use, Red Light Therapy provides a gentle yet meaningful way to encourage healthier, more comfortable skin, an empowering step for those navigating the ongoing challenges of eczema.
References:
[1] Tian J, Zhang D, Yang Y, Huang Y, Wang L, Yao X, Lu Q. Global epidemiology of atopic dermatitis: a comprehensive systematic analysis and modelling study. Br J Dermatol. 2023 Dec 20;190(1):55-61. doi: 10.1093/bjd/ljad339. PMID: 37705227.
[2] Hottz F, Herchenhorn D, Lenzi J, Andrade J, Freire V, Pinho P. Photobiomodulation as a treatment for dermatitis caused by chemoradiotherapy for squamous cell anal carcinoma: case report and literature review. Radiat Oncol. 2022 Mar 7;17(1):49. doi: 10.1186/s13014-022-02015-4. PMID: 35255933; PMCID: PMC8903640.
[3]Lin YT, Tung KM, Chiou JF, Chen YC, Hou WH. Effects of photobiomodulation therapy for acute radiation dermatitis in patients with cancer: A systematic review and meta‑analysis of real-world evidence. Radiother Oncol. 2025 Jan;202:110589. doi: 10.1016/j.radonc.2024.110589. Epub 2024 Oct 18. PMID: 39426526.
[4]Strouthos I, Chatzikonstantinou G, Tselis N, Bon D, Karagiannis E, Zoga E, Ferentinos K, Maximenko J, Nikolettou-Fischer V, Zamboglou N. Photobiomodulation therapy for the management of radiation-induced dermatitis : A single-institution experience of adjuvant radiotherapy in breast cancer patients after breast conserving surgery. Strahlenther Onkol. 2017 Jun;193(6):491-498. English. doi: 10.1007/s00066-017-1117-x. Epub 2017 Feb 27. PMID: 28243723.